What is Mast Cell Activation Syndrome?
Everything you need to know about MCAS
Photo by Jamie Street on Unsplash
What is Mast Cell Activation Syndrome?
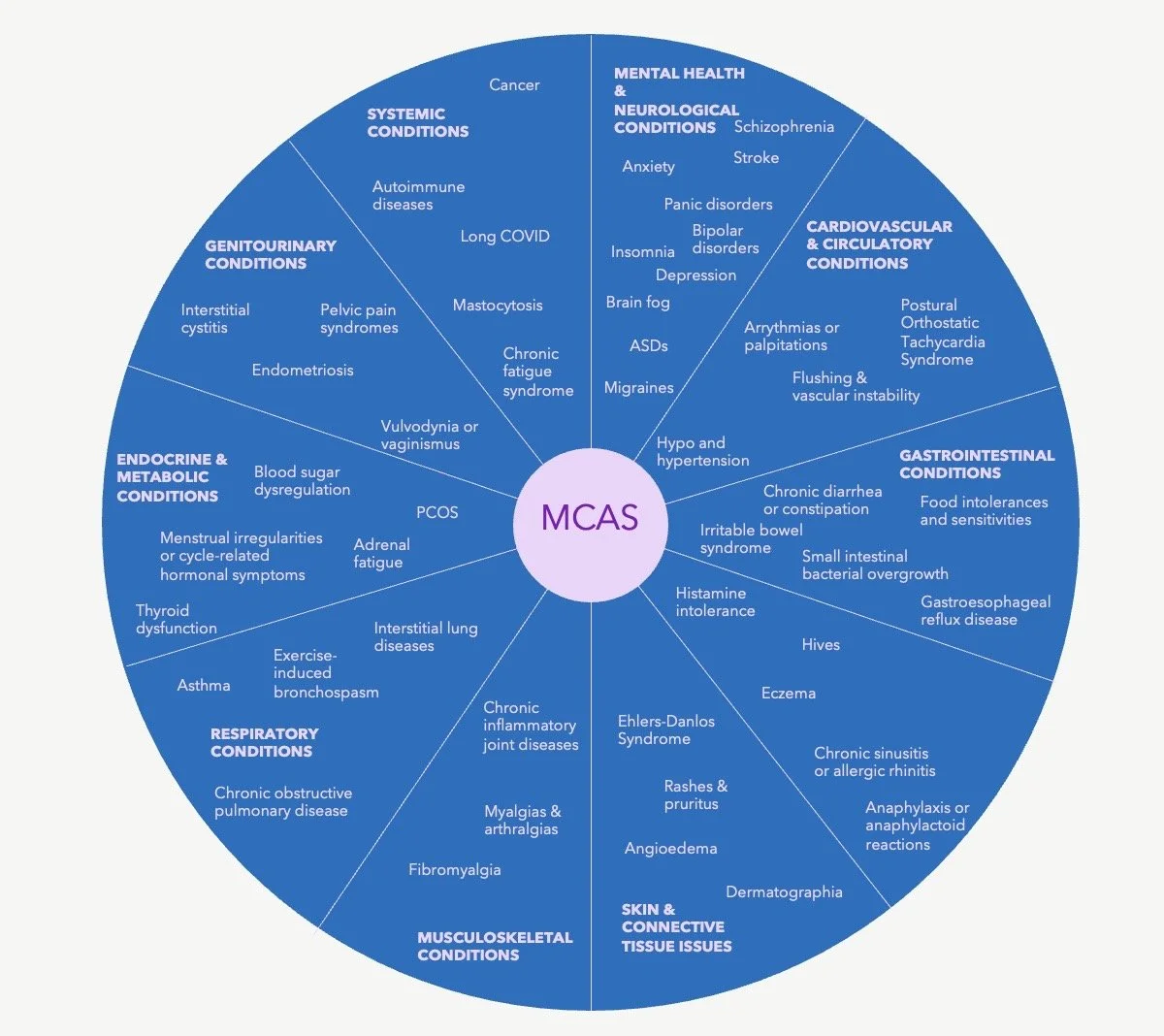
If the picture above inspires dread and thoughts of hay fever or allergies in you, then you may have Mast Cell Activation Syndrome (MCAS). MCAS occurs when mast cells, immune cells found in tissues such as the skin, gastrointestinal tract, and respiratory system, become overly reactive and release excessive amounts of their chemical mediators. These mediators, including histamine, tryptase, prostaglandins, leukotrienes, and cytokines, play crucial roles in inflammation and allergic responses. Because inflammation can act as a driver of so many chronic health conditions, MCAS has been implicated in a wide range of health conditions beyond allergies and hay fever. These range from hypertension and cardiovascular issues to cancer and autoimmune diseases. A comprehensive grouping of issues linked to MCAS is provided in the diagram below.
MCAS has been implicated in a wide range of chronic health issues, all of them inflammatory conditions.
How can mast cells be involved in so many different conditions? In normal circumstances, mast cells respond to threats like allergens or infections, releasing these chemicals to help the body fight off invaders or heal injuries. However, in MCAS, mast cells release these substances inappropriately, often in response to triggers that wouldn't typically provoke such a response.
The release of these mediators can lead to a cascade of symptoms. Histamine, for example, is involved in itching, flushing, swelling, and gastrointestinal issues, while prostaglandins and leukotrienes contribute to inflammation, bronchoconstriction, and pain. Tryptase, an enzyme specific to mast cells, can cause tissue damage and exacerbate inflammation. These substances affect nearly every organ system, which is why MCAS symptoms are so varied, ranging from mild allergic-type reactions to issues with heart health and cognitive dysfunction. This dysregulated mast cell activity leads to chronic inflammation and can disrupt homeostasis, causing significant physical and mental health challenges.
Triggers for mast cell activation in MCAS include environmental allergens, certain foods, stress, infections, or even temperature changes. The unpredictability and range of symptoms make MCAS a complex condition to diagnose and manage.
What are mast cells?
Mast cells are immune cells found in tissues like the skin, lungs, and gut, particularly in areas exposed to the outside world. They’re part of the body’s first line of defence, responding to things like allergens or infections. These cells store chemicals such as histamine, cytokines, and prostaglandins, which they release when triggered. This release helps create inflammation, recruit other immune cells to the site of a threat, and even aid in tissue repair. While this process protects the body, it’s also what causes the symptoms of allergic reactions like swelling, itching, and redness.
Mast cells also play a role in connecting the body’s innate and adaptive immune systems, helping to strengthen long-term immunity. They assist in activating dendritic cells (which help identify pathogens) and support T and B cells in creating specific immune responses. This makes mast cells key players not just in allergy and inflammation but also in shaping the body’s ability to recognise and fight specific threats over time.
What are symptoms of Mast Cell Activation Syndrome?
The severity and combination of symptoms of MCAS vary between individuals, but they are both typically chronic (long-term) and episodic (more severe at times). They are often triggered by factors such as stress, food, environmental allergens, or infections.
Skin Symptoms:
Flushing
Hives (urticaria)
Itching (pruritus)
Swelling (angioedema)
Gastrointestinal Symptoms:
Abdominal pain
Diarrhoea or constipation
Nausea and vomiting
Food intolerances or sensitivities
Respiratory Symptoms:
Wheezing or asthma-like symptoms
Nasal congestion
Throat swelling or tightness
Cardiovascular Symptoms:
Low blood pressure (hypotension)
Dizziness or fainting
High blood pressure (hypertension)
Heart disease
Rapid or irregular heartbeat (tachycardia, palpitations)
Neurological and Psychological Symptoms:
Brain fog or difficulty concentrating
Headaches or migraines
Anxiety or irritability
Depression or malaise
Autism Spectrum Disorders
Bipolar disorder
Schizophrenia
Systemic Symptoms:
Chronic fatigue
Muscle or joint pain
Sensitivity to temperature changes
Anaphylaxis (severe systemic allergic reaction in extreme cases)
In addition, evidence is emerging that MCAS may be involved in tumour development and progression.
Since MCAS symptoms overlap with many other conditions, such as irritable bowel syndrome (IBS), chronic fatigue syndrome, and fibromyalgia, diagnosis often requires ruling out other causes.
Getting a Diagnosis for Mast Cell Activation Syndrome
Diagnosing MCAS involves a mix of clinical assessment, lab tests, and sometimes genetic testing. Symptoms like flushing, gastrointestinal upset, or respiratory issues that come and go in response to triggers (e.g., stress, allergens, or foods) are an important starting point. The focus is on identifying mast cell overactivation through specific markers and ruling out other possible conditions.
Key Diagnostic Steps
Clinical Symptoms: A history of episodic symptoms involving multiple systems (like skin, gut, and cardiovascular) suggests mast cell activation. Symptoms often flare in response to triggers.
Lab Tests During Flares:
Tryptase Levels: A significant rise from baseline (20% + 2 ng/mL) is a strong indicator but isn’t always elevated in MCAS.
Urine Tests: These check for high levels of substances like histamine metabolites and prostaglandin D2, key indicators of mast cell activity.
Plasma Histamine: Measuring histamine levels during symptoms can support the diagnosis but is less consistent.
Response to Treatment: If symptoms improve with antihistamines or mast cell stabilisers, it supports the diagnosis.
Genetic Testing: Testing for AOC1 (diamine oxidase) and HNMT (histamine-N-methyltransferase) genes can help identify issues with histamine breakdown. DAO mainly works in the gut, breaking down dietary histamine, while HNMT breaks it down in tissues. Mutations in these genes may worsen histamine-related symptoms, though they don’t confirm MCAS directly.
Excluding Other Conditions: Diagnosing MCAS involves ruling out conditions like mastocytosis (which is when there are excess mast cells in the body), histamine intolerance (although the two often overlap), and other allergies. This process is critical to avoid misdiagnosis.
In saying that, MCAS can be incredibly difficult to diagnose because the biomarkers used in diagnosis are not necessarily always present in the body. They need to be measured within four or so hours following a known reaction in which mast cells have released inflammatory mediators. Cross-referencing against symptoms is therefore also considered a valid diagnostic approach.
Causes of Mast Cell Activation Syndrome
MCAS often develops due to a mix of genetic, environmental, and lifestyle factors that influence mast cell behaviour. While the exact causes are not fully understood, underlying triggers include genetic predispositions, such as mutations in mast cell regulatory genes, chronic infections, and immune system dysregulation. These factors can lead to overactive mast cells releasing inflammatory chemicals, causing the wide array of symptoms seen in MCAS.
Mitochondrial dysfunction has been implicated as a contributing factor in MCAS. Mitochondria, the energy powerhouses of cells, also regulate immune responses. When mitochondria don’t function well, it can lead to increased oxidative stress and inflammation, which can worsen mast cell overactivation. Chronic stress further exacerbates this, as it elevates cortisol and other stress hormones that influence mast cell activity. Long-term stress may dysregulate the nervous system and make mast cells more reactive to triggers.
Nutrient deficiencies, such as low levels of vitamin D, magnesium, and antioxidants, may also play a role in MCAS. These nutrients are essential for proper immune regulation and reducing oxidative stress. For instance, vitamin D helps balance the immune system, while magnesium is important for stabilising mast cells and reducing their overactivation. Lifestyle factors such as a nutrient-poor diet, emotional stress, poor gut health, lack of sleep, too much or too little movement, and an environment laden with chemicals or pathogens (mould can play a major role here) can deplete these nutrients and worsen symptoms.
Treatment of Mast Cell Activation Syndrome
Treating Mast Cell Activation Syndrome (MCAS) involves tailoring approaches to address its underlying triggers, which can include allergies, infections, chronic stress, or nutrient imbalances. For instance, antihistamines or mast cell stabilisers may be used to reduce symptoms in the short term, while dietary changes, stress management, or gut health improvement may address root causes over time. However, regardless of the specific triggers, stabilising mast cells requires focusing on improving mitochondrial function and maintaining a healthy redox balance—the balance between antioxidants and free radicals in the body.
Mitochondria are vital not just for energy production but also for controlling inflammation and oxidative stress. Dysfunctional mitochondria can amplify mast cell reactivity, leading to more symptoms. By supporting mitochondrial health through strategies like eating an antioxidant-rich diet, reducing oxidative stress, targeting specific nutrient deficiencies and imbalances, and managing chronic stress, the body can achieve better immune balance. This approach helps stabilise mast cells at their core and promotes long-term symptom relief.
Can you live a normal life with Mast Cell Activation Syndrome?
Yes! MCAS is a tricky condition, but once the underlying cause of the issues have been identified and are addressed, mast cells can re-stabilise. While the genetic predisposition and sensitivity to stressors will always be there, by looking after yourself and managing stressors and triggers, you can indeed return to a normal, healthy life.
The more you learn about MCAS and its symptoms and what has caused it for you, the better you’ll get at recognising when something is triggering a reaction and taking you outside your window of tolerance. You can then work to remediate these stressors and bring yourself back into your window of tolerance, either through reducing stressors or by ensuring that your body is fully supported to deal with whatever demands you’re placing on it.
Did you know that I have an entire course - with over 20 hours of video learning - on MCAS? It helps you not only understand the underlying cause of MCAS symptoms but also what’s driving them and what you can do to reverse it. Plus you get a free practitioner consult to make sure you’re on the right track to reverse your MCAS. Learn more or sign up by clicking the button below.